Transforming Rural Health Care: A Roadmap for Collaboration and Change
By Ashley Antonelli
/ February 16, 2024
At Health Evolution’s 2023...
Read More
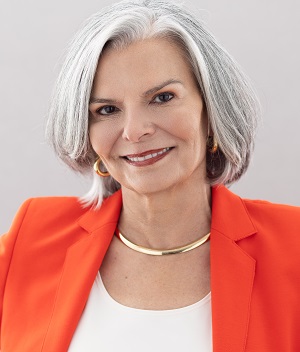
Revolutionizing Mental Health Support: A Strategic Imperative for Health Care CEOs
By Ashley Antonelli
/ January 29, 2024
At the forefront of...
Read More
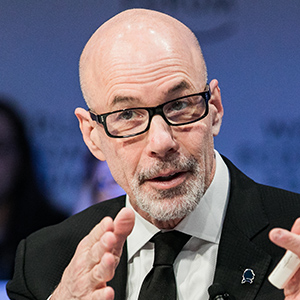
The Golden Rule in Health Care Leadership: An Interview with Amedisys’ Paul Kusserow
By Health Evolution
/ January 22, 2024
Health Evolution CEO Richard...
Read More
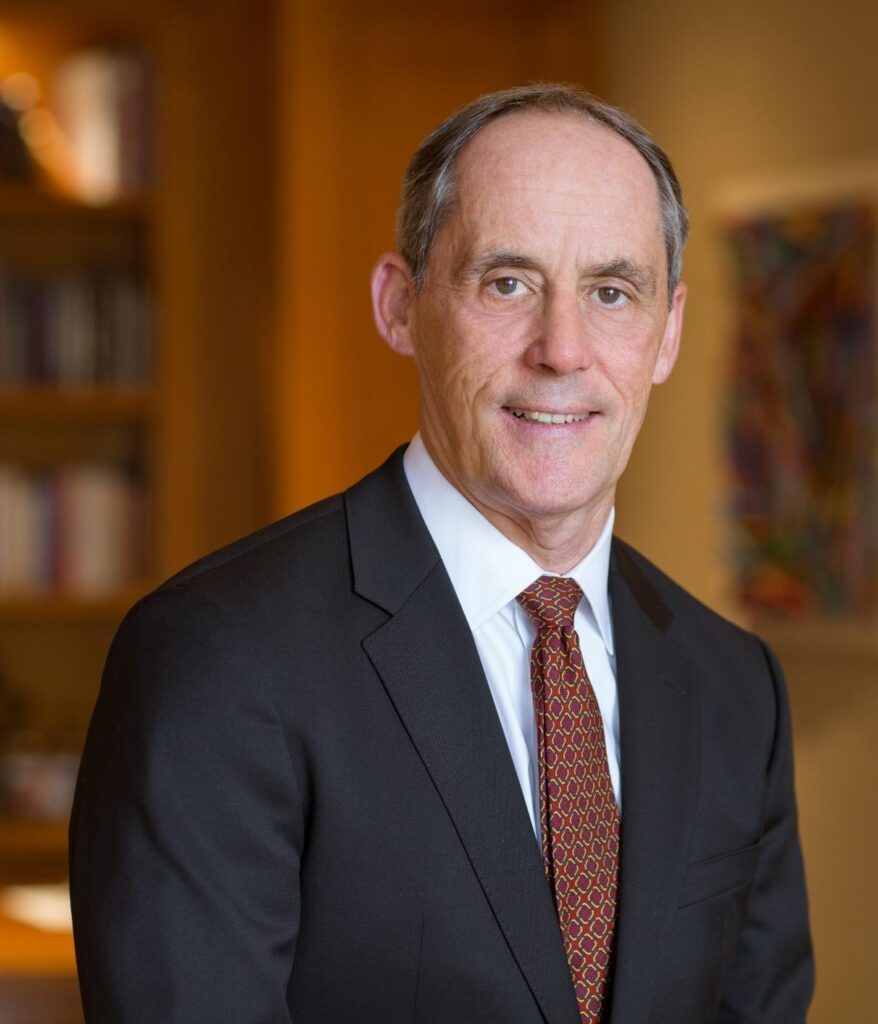
Leadership Profile: Sutter Health’s Tosan Boyo
By Health Evolution
/ December 14, 2023
Tosan Boyo is the...
Read More
Health Evolution Data Trust Framework Serves as Basis for New Joint Commission Certification Program
By Ashley Antonelli
/ December 5, 2023
Health Evolution is excited...
Read More
Leading an AI-Powered Future: What Health Care Executives Need to Know
By Ashley Antonelli
/ November 30, 2023
AI’s dramatic impact has...
Read More
Measuring Outcomes in Mental and Behavioral Health: Insights from Health Evolution’s Roundtable on Innovations in Mental and Behavioral Health
By Ashley Antonelli
/ November 27, 2023
As rates of unmet...
Read More
‘Something Drastic Needs to Change’: Reimagining a New Future for Specialty Care
By Ashley Antonelli
/ November 15, 2023
Primary care long has...
Read More
‘Be Relentless’: How to Lead and Advance Health Equity Amid Rising Polarization and Politicization
By Ashley Antonelli
/ November 9, 2023
Across the past two...
Read More