While the pandemic itself continues to disrupt American life, the dust has settled on the initial wave of telehealth usage during COVID-19.
The Bipartisan Policy Center, with assistance from market research firm SSRS, released a survey of nearly 2,000 patients that aimed to determine utilization rates of consumer telehealth during the pandemic. Nearly one-third of American adults had a telehealth visit for themselves or a dependent in the last year, according to the survey.
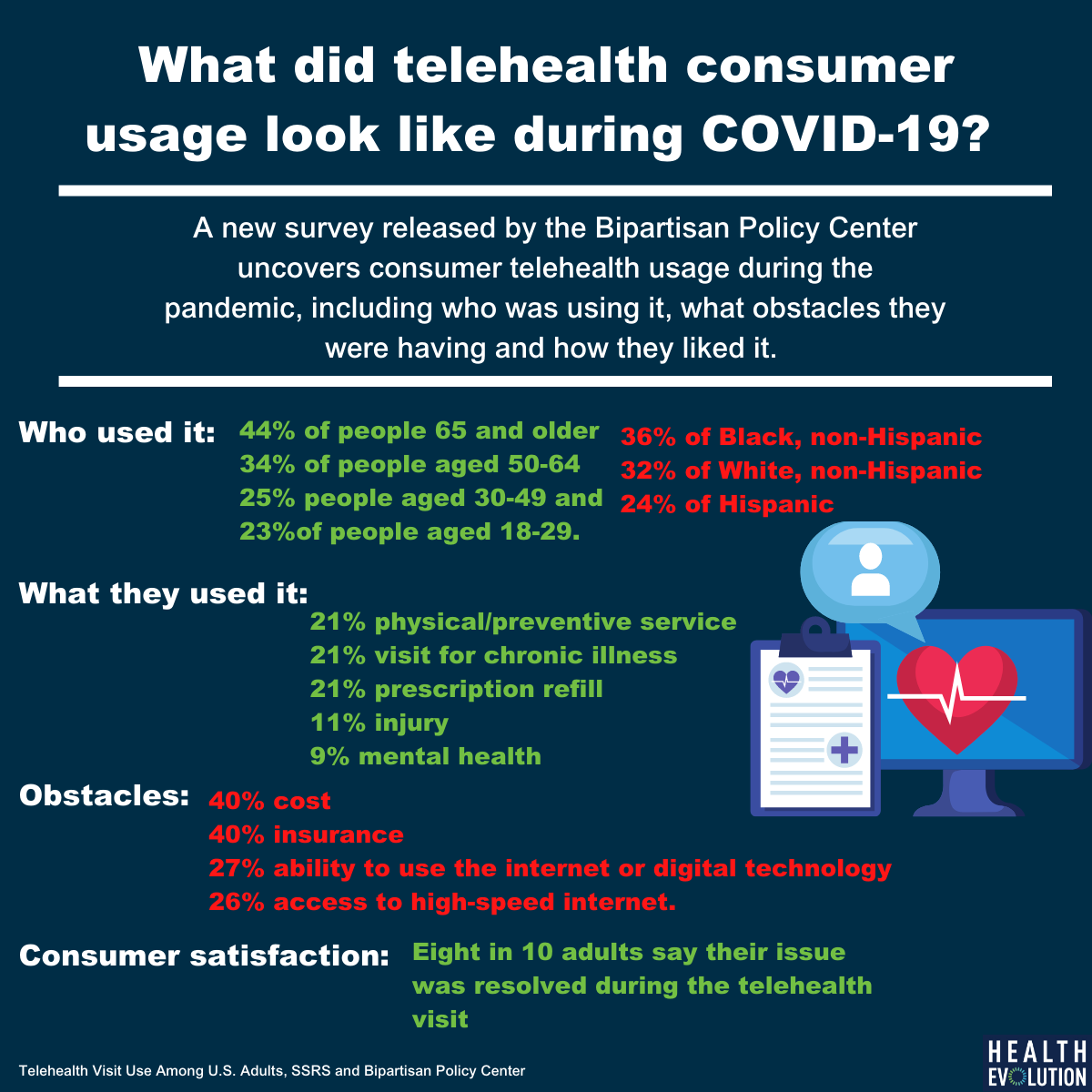
This usage included 44 percent of Medicare beneficiaries, 34 percent of people aged 50-64, 25 percent of people aged 30-49 and 23 percent of people aged 18-29. According to the survey, 36 percent of Black Americans used telehealth, 32 percent of White Americans and 24 percent of Hispanics. Roughly 31 percent of those with employer-sponsored insurance accessed care virtually and 34 percent of rural residents, compared to 11 percent of uninsured people and 31 percent of non-rural residents.
Dorothy Siemon, senior vice president of the office of policy development and integration at AARP, wasn’t surprised to see growing interest in telehealth from Americans aged 50 and older. “There is a lot of interest from people that age in engaging with telehealth. It can make things more convenient. There are benefits to family caregivers. They see the promise of this convenience,” said Siemon during a recent Bipartisan Policy Center webcast.
Challenges in tech, access for older Americans
In terms of what telehealth people used, the mix between audio and video visits was split. In total, 51 percent of visits were conducted via video and 43 percent were done using audio. People aged 65 and older leaned more towards audio visits with 47 percent engaging in that modality while 44 percent used video. Interestingly, 7 percent indicated that they didn’t remember whether the virtual visit was based on audio or video. According to Siemon, audio is important for older Americans who don’t have access to broadband or digital devices, especially in rural areas.
According to the survey, 45 percent of patients say that technology is an obstacle to receiving care via telehealth. This includes 27 percent who say their ability to use the internet or digital technology is an obstacle and 26 percent say it’s access to high-speed internet. These problems impact 35 percent of rural residents compared to 26 and 24 percent of non-rural residents. It’s even more pronounced of a challenge for older Americans. The survey found that 49 percent of older adults say using digital technology is an obstacle, 42 percent have trouble accessing high-speed broadband internet and 46 percent can’t easily get to a computer/video device.
“There are more people across the ages who need help with digital training. We need to meet people where they are. If this is truly health access then we need to meet older—and all people—where they are,” Siemon said. “We need to invest in broadband and tech support so all populations, particularly older people, can access this. Audio is sometimes the only way they can get to the clinician they need.”
Recently, more than 400 health systems, associations and stakeholders wrote a letter to Congressional leaders requesting that they permanently address many of the temporary telehealth measures enacted during the pandemic. One of their chief priorities is to equip federal-qualified health centers, critical access hospitals and other safety-net providers with the tools and reimbursement needed to leverage telehealth. The bipartisan Infrastructure Bill would set aside $65 billion to expand broadband internet in underserved areas.
It wasn’t just technology that held back telehealth usage for patients during the pandemic’s first year. Cost and insurance coverage were the biggest obstacles for 40 percent of patients surveyed, including 56 percent of Black Americans and 45 percent of Hispanic Americans.
Consumer feedback
Overall, the most common reasons for telehealth visits were preventive service, prescription refill, or routine visit for chronic illness, according to the survey. For rural residents, the primary usage of telehealth was for surgical consults and non-rural residents used it for prescription refill. Kate Goodrich, MD, senior vice president of analytics and trends at Humana, says the insurer saw its members use the technology primarily for chronic care with their own doctors.
“We re-oriented our care management work inside Humana to identify our members most at risk for hospitalization and not being able to get refills,” said Goodrich during the webcast. “We made a particular effort to reach out to members who have greater social needs and if they had great physical needs, to work directly with them to access their own physician or clinician. What we saw during the early months of the pandemic is the vast majority of our members used telehealth with their primary care physician and not with a vended solution.”
Goodrich says that providers in a value-based contact were more likely to use telehealth than those using fee-for-service reimbursements. She says many of these people had telehealth capabilities in place before the pandemic, and if they didn’t have one, value-based providers worked hard to stand up a telehealth platform.
The survey also found that patient satisfaction with telehealth was strong. Eight in 10 adults say their issue was resolved during the telehealth visit, including 96 percent of people seeking a prescription refill, 82 percent of people using it for a routine chronic illness visit, and 80 percent of people using it for an annual physical or preventive service. In total, there was a 94 percent satisfaction rate with telehealth among all patients that stayed consistent through the different ages, locations, and insurance types.
“People, providers and patients, when given the opportunity, use telehealth and they like it. And what’s interesting is when telehealth is not offered, people said they would have used the emergency room, which is very expensive, or they would have skipped care altogether, which is also expensive down the road. This is something we’ve exposed and it underscores the importance of making those changes we’ve seen become permanent,” said Ann Mond Johnson, CEO of the American Telemedicine Association during the Bipartisan Policy Center webcast.