In this series, Health Evolution is examining the year 2021 in health care through the lens of our eight imperatives. We will be examining the trends that were at the top of CEOs’ minds throughout the past year and what may come in 2022. This week: Escalating Health Equity
Previously:
The status of health disparities in America was made worse by the COVID-19 pandemic. The struggles that started in 2020 have continued to escalate in 2021.
In a new wide-ranging report, the Commonwealth Fund found that the average life expectancy of Black, Hispanic, and American Indian/Alaska Native people fell more sharply during the pandemic than those of White people. These populations are also “less likely to have health insurance, more likely to face cost-related barriers to getting care, and more likely to incur medical debt,” according to the report. They also are more likely to live in poverty, work in low-paying, high-contact industries, and to reside in high-risk living environments. In every state studied by the Commonwealth Fund, there were disparities. Even in the states where minorities scored above the national average, they still trailed White people in outcomes.
“The U.S. health care system is not immune from the systemic inequities that plague American society. Our health care is characterized by long-standing disparities in access, quality, and outcomes for people of color that were unveiled for many by the COVID-19 pandemic. We can do better, and we can start by tackling systemic racism, ensuring people have the health care coverage they need, and resolving racial disparities in care,” said study co-author Laurie Zephyrin, MD, Commonwealth Fund Vice President for Advancing Health Equity.
These are the challenges that health care CEOs in every corner of the industry are trying to address in some way, shape or form. Earlier in 2021, leaders of Health Evolution Forum’s Work Group on Leveraging Data to Improve Health Equity, which includes Zephyrin, received commitments from more than 40 leading organizations to collect, stratify and review race, ethnicity, language, and sex data (REaLS) data.
Learn more about the Health Equity Pledge here.
Beyond the use of data, health disparity-related initiatives and research efforts have taken hold across the industry. Much of it has come in the form of addressing the social determinants of health, a somewhat controversial phrasing that encompasses factors influencing the health of individuals and populations, such as socioeconomic status, housing, zip code, transportation, education levels, employment and health insurance, food insecurity and others.
A recent survey from Mercer found that nearly half of all large employers – and about two-thirds of those with 20,000 employees — say that addressing health equity and the social determinants of health will be an important priority over the next 3-5 years. A report from NORC at the University of Chicago found that Medicare Advantage plans are increasingly investing in social determinants of health benefits. An analysis of 57 health systems in Health Affairs found that they were spending billions on programs addressing housing and employment, and hundreds of millions on education, food security, and community context.
FarmboxRx CEO Ashley Tyrner has created a program that allows patients to use over-the-counter benefits to purchase curated boxes of produce that are tailored to chronic conditions and delivered to patients’ homes nationwide. With more than 50 health plan partners signing on to this plan (up from three plans in one year), the shift has been successful enough that FarmboxRX is cutting back on sending produce boxes directly to consumers.
“We spend an estimated $53 billion annually on diet-related chronic conditions. We cannot sustain that, right? That number is continuing to grow year on year. So, health plans are desperate to make changes to their members’ health and instead of treating the member repetitively with prescriptions and medications that can cause other problems and mask the underlying problem, which is a chronic related diet condition, they are looking at nutrition and there’s a shift in the market,” Tyrner says.
Communication and trust
Those working to reduce health disparities say that communication and trust are two of the biggest barriers they face on a consistent basis. In the Twin Cities in Minnesota, Axis Medical Center, a federally qualified healthcare center (FQHC), serves primarily an immigrant patient population with one foot in America and one foot in another nation, says Jonathan James, MD, Axis’ chief financial officer and an epidemiologist. More than half of Axis’ patients live at or below the poverty line and more than 80 percent are best served in a language other than English.
“These people have some difficulty navigating the health system simply by the barrier of language,” says James. There are also cultural difficulties, he notes. “Most of them have never seen snow. They arrive in Minnesota in the dead of winter without a jacket and it’s 3 degrees outside.”
To deal with the language barriers, Axis employs international medical graduates who can interpret for these patients. This doesn’t just allow for patients to understand what the clinician is trying to tell them, but it makes them feel more at ease, James says. “They see someone who looks like them and speaks their language. It resonates when that person can tell [the patient], ‘Yes I understand. I know where you’re from. I’m from there too.’ There is a confidence and trust that’s built,” James says.
We’re not able to humble ourselves. In so many ways we get it wrong because we think we know better. We went to school. We know what this is. We get it wrong when we stop listening to the patient.
Jonathan James, MD, Axis Medical Center, chief financial officer and an epidemiologist.
Trust is incredibly important when reaching underserved populations, he notes. Many of their patients are leery of government agencies and the health care system in general. “We have made a concerted effort to walk in the community and meet people one-on-one, talk to them and try to break down some of those barriers,” James says.
This has been especially the case during COVID, as misinformation has spread like wildfire in underserved communities where vaccine rates are still lagging even though some inroads have been made, according to a Kaiser Family Foundation analysis. Moreover, James says the spread of COVID happened much more rapidly in these communities because of a lack of access to transportation, healthy food, and housing security. He says often times families of 8-10 people live in close quarters and cram into cars because it’s the only transportation they have available.
Access to specialty care
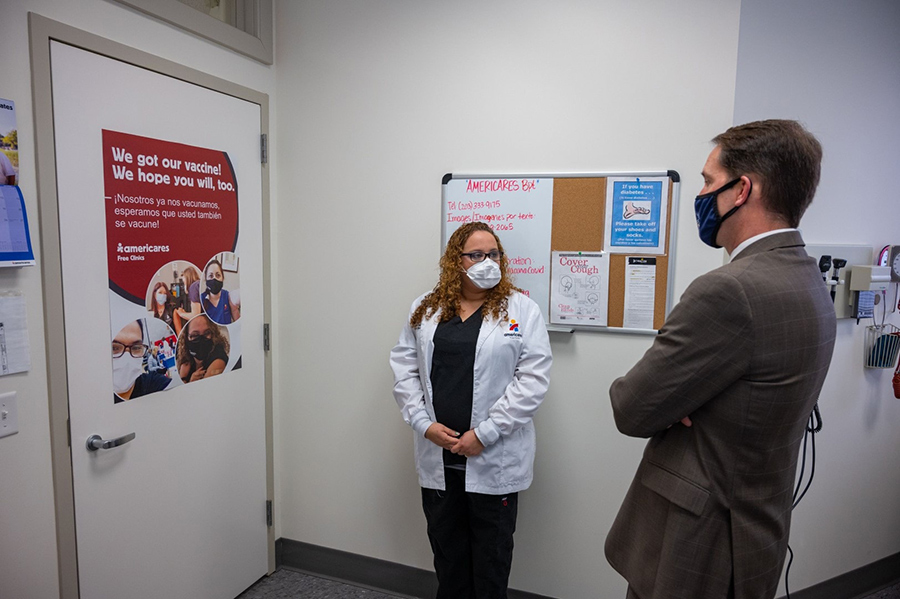
Americares Free Clinics provides care to uninsured patients in Western Connecticut. For its Stamford-based clinic, nearly 90 percent of the patients and almost everyone who works at the clinic is Latino. This connection allows workers to communicate effectively with patients from a cultural perspective to get them to engage in healthier eating, says Karen Gottlieb, executive director of Americares Free Clinics. “It’s not to change their diet, it’s to teach them within their cultural norms to help control their diabetes,” Gottlieb says.
But while communication isn’t as big of a challenge, access to specialized care is a problem for this patient population, she says. “Because of the nature of our patients’ chronic disease, primary care is often not enough,” says Gottlieb. She says the clinic leverages community partnerships to serve these patients’ specialty care needs. “Volunteers will see our patients in their offices at no charge, and all the hospitals have specialty clinics that we can refer our patients to. We’re trying our best to get our patients access to that specialty care and we have to be creative about it.”
The clinic also uses telehealth to access specialty care providers, which is a mechanism that has been prominently utilized since the start of the pandemic, Gottlieb says. In fact, from March 16 to August of 2020, almost all patient encounters were done virtually. She says the clinic did a lot of hand holding to bring patients up to speed on telehealth during the pandemic to ensure they had continuous access to care and were safe from exposure to the virus. From August 2020 onward, the clinic employs a hybrid model of care, and telehealth has been embraced by patients.
“Patients like the idea that they don’t have to miss a whole day of work to get transportation to come into a clinic. They can pick up the phone for a 15-minute call. They work at Wendy’s and can walk outside to take a call. They’re a landscaper, they can put down their equipment and step aside. Telehealth is here to stay as a modality of care,” Gottlieb says.
One of the biggest misconceptions about undeserved populations, particularly those who are uninsured, is that they don’t care about their health, Gottlieb says. “Our patients are very interested in staying well. They are interested in maintaining their health. When they come to the clinic and are shepherded through treatment plans, they are nothing but grateful and for the most part, they’re adherent to the regimens prescribed,” she says.
Stay humble
James agrees with Gottlieb’s assessment on underserved patient populations’ desire to stay healthy—and the misconception that they don’t care. He says that neglect comes not from apathy, but from the social determinants of health and the inability to access care.
“In this population, over and over again neglect becomes a Petri dish of disease. Unaddressed health concerns that could be remediated aren’t because they don’t have access to care, don’t know about it, can’t get there, or there’s a barrier of language. We have far too many patients that if they had been connected with good medical care earlier, they would not be suffering today,” James says.
Like James and Gottlieb, Tyrner at FarmboxRX says there is a misconception that underserved patient populations don’t want to eat healthy or go to the doctor. Often, they don’t have access, nor do they understand the benefits available to them, she says. As such, health plans don’t just use Farmbox’s healthy food boxes to improve their diets, but also as a way to engage patients and educate them on their benefits.
“On a health equity level, education is vital in being able to speak to your membership to understand the benefits they have available to them,” Tyrner says. Addressing SDOHs should also be done holistically, she adds, as those with housing insecurity may have transportation and food challenges as well. Health care organizations are only starting to understand this about addressing SDOHs, she adds.
All told, this lack of understanding goes back to what James says is the most common problem he sees in how health care organizations try to tackle disparities: They don’t listen to the patients. They don’t try to solve the patients’ challenges without consulting the patient themselves, which he says is disrespectful and leads to that mistrust of the system.
“We’re not able to humble ourselves. In so many ways we get it wrong because we think we know better. We went to school. We know what this is. We get it wrong when we stop listening to the patient. We get it wrong when we don’t have a fundamental concern for the humanity of people,” says James.