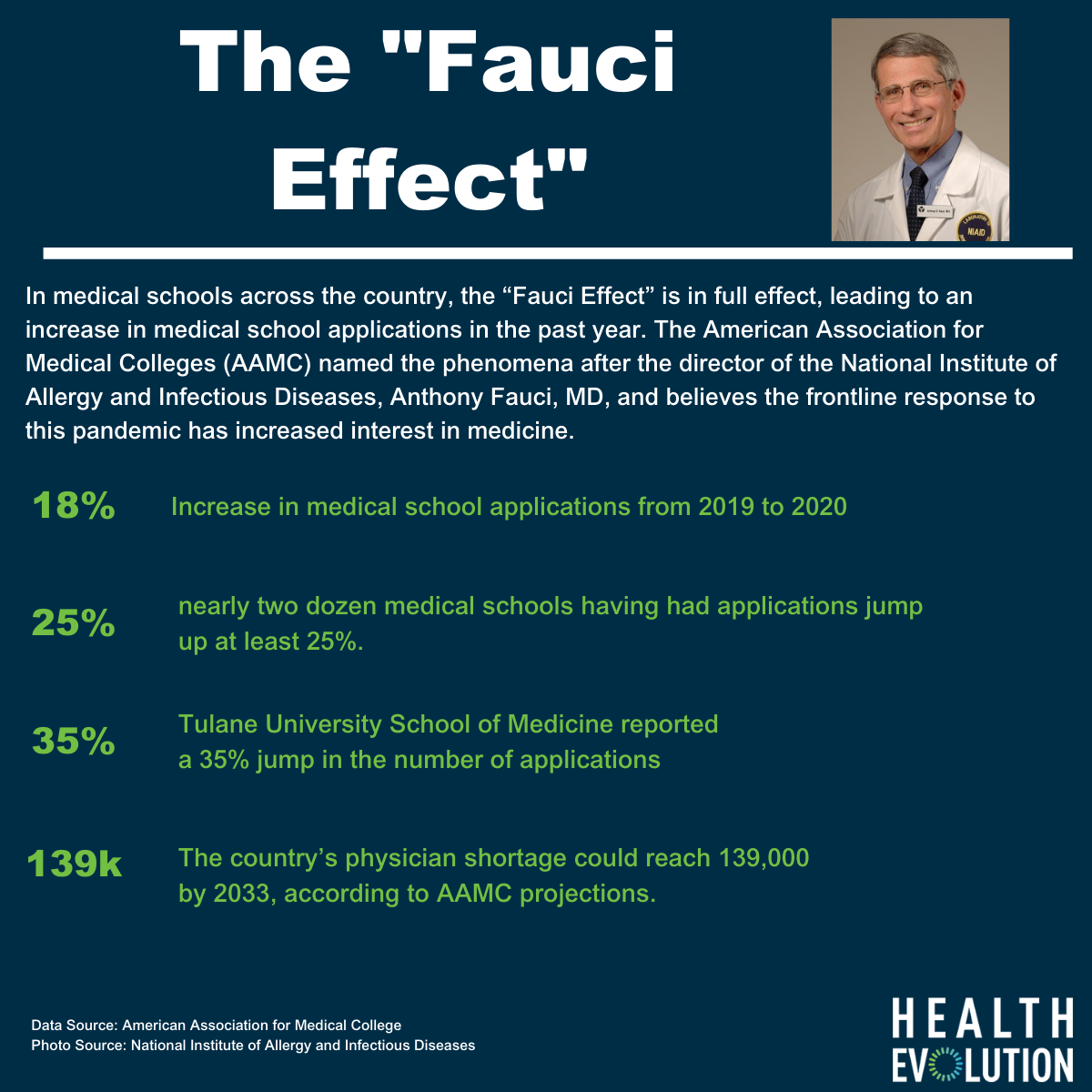
In medical schools across the country, the “Fauci Effect” is in full swing, leading to an increase in medical school applications in the past year. American Association for Medical Colleges (AAMC) says there has been an 18 percent increase in year-over-year medical school applications, with nearly two dozen medical schools having seen applications jump up at least 25 percent.
The association named the phenomena after the director of the National Institute of Allergy and Infectious Diseases, Anthony Fauci, MD, and believes the frontline response to this pandemic has increased interest in medicine. “I make an analogy to the time after 9/11, when we saw an increase in those motivated to serve this country militarily,” said Geoffrey Young, PhD, AAMC senior director for student affairs and programs. “This certainly seems like a significant factor this year.”
According to NPR, Stanford University School of Medicine reported a 50 percent jump in the number of applications, while Boston University School of Medicine reported applications are up 26 percent and Tulane University School of Medicine in New Orleans reported a 35 percent increase compared to the same time last year. These increases come as the country’s physician shortage could reach 139,000 by 2033, according to AAMC projections.
Web-side manner training
The increased interest in medical school may be an opportunity to help guide future doctors in virtualized care, says Rafid Fadul, MD, Executive Medical Officer at Wheel and the Director of Pulmonology at the Blanchard Valley Health System, part of the Mayo Clinic Care Network. As someone who lives two lives, one at a telehealth company and one in the traditional brick-and-mortar care settings, he has seen the pandemic’s impact on the adoption of telehealth firsthand.
“The late adopters finally started to adopt. A lot of my colleagues realized technology can be used to enhance their performance and it wasn’t just a stopgap for COVID. It had a lot of value to monitoring patients and in improving care overall,” Fadul says. It goes beyond two-way video. For instance, as a pulmonologist, he can monitor how many times a patient is taking their rescue inhaler.
With more acceptance in medicine for technology, Fadul says now is the time for educators to help providers navigate this new reality. He says medical schools should help providers understand how to triage and direct patients virtually. The technology isn’t meant for everyone and each encounter will open up a slate of questions that could send patients off in the wrong direction. He also says education must account for the fact that providers and patients aren’t in the same room during these encounters.
“We have to find ways to build trust and rapport with a patient, even though they may not be in the same room. That’s about web-side manner—the patient has trust in the person providing their care. The setting is professional. Their attire is professional,” Fadul says. And then once that trust is established, providers must be trained on how to hone their observational skills in a virtual setting. “Is there a slight tremor? Is there a slight jaundice in the eyes? These are the subtle findings we have to tease out.”
Where telehealth and medical school come together
When the American Medical Association called for an incorporation of telemedicine training into medical school in 2016, many institutions responded. According to AAMC, half of all medical schools offered a telehealth course either as a requirement or elective in 2017. The courses can help make more doctors accepting of the practice. In a study done by researchers at the Uniformed Services University of the Health Sciences, 80 percent of medical students who were given telehealth training indicated future plans to use the technology in practice.
Many schools used the pandemic to jump start their efforts. At UMass Memorial Medical Center, Amwell trained third and fourth-year medical students on the nuts and bolts of telehealth in the early days of COVID-10 to allow them to help out as needed. Harvard Medical School has made practicing telemedicine skills to students a priority since the pandemic began and integrated it into the curriculum. The school created a five-module telemedicine course that covered what telemedicine is, the ethical issues are around it, and to how to set up successful tele-visits.
“How do you do a virtual visit, and then how do you engage a student in a virtual visit so they can really learn things? There are really two aspects. We’re doing this in parallel. We’re teaching the students, and we’re also having to teach the faculty and figure it out ourselves,” Barbara Cockrill, MD, the Harold Amos Academy Associate Professor at Harvard Medical School and Brigham and Women’s and Director of Faculty Development at Harvard Medical School said to The Harvard Gazette.