The Supreme Court’s impact on the health policy landscape has been notable in the last few years with rulings on the Affordable Care Act and COVID-19-related mandates, but a lesser-known case argued in late November could have just as important of an impact on the power of HHS and other agencies.
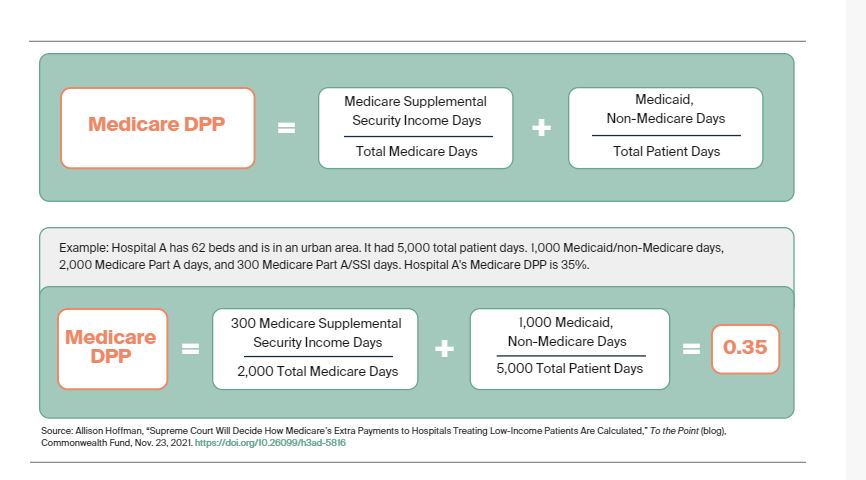
Becerra vs. Empire Health Foundation could have a downstream impact on how agencies are able to issue rules based on their interpretation of statutes. At issue in this case is a rule HHS issued in 2005 changing the way it calculated the annual reimbursement rate paid to hospitals by the Medicare program for treating low-income patients, often called a disproportionate share hospital (DSH) adjustment. According to the Commonwealth Fund, DSH payments are calculated the following way:
The legality of HHS interpretation of these payments comes down to the words “entitled to,” and “eligible to,” when calculating these payments. According to SCOTUS Blog, HHS’ regulation made it so the “entitled to” definition under the Medicare portion of this calculation included “all patients legally entitled to receive Medicare benefits, regardless of whether Medicare actually paid the hospital bills of those patients.” Because this includes all the patients who were entitled to Medicare benefits, it significantly cut Medicare payments to safety-net hospitals.
Health Evolution Summit 2022, April 6-8, Laguna Niguel, CA: Apply to Attend
Empire Health Foundation, which owned a safety-net hospital that was impacted by these rules, challenged HHS’s authority to make that interpretation. Empire essentially said the law would have said “eligible to” if it wanted to include everyone eligible for Medicare benefits. The Ninth Circuit ruled against HHS in 2020 affirming the decision of a district court.
Far-reaching impact
On the surface, it would seem this case would only impact safety-net hospitals and those with a large share of low-income patients. However, Robert Bradner, an attorney at the law firm Holland & Knight’s Federal Practice with broad experience in health care policy and funding, says that this ruling could have a far-reaching impact.
“The Supreme Court is wrestling with to what extent they should be scrutinizing regulations. You hear the word deference—to what extent should a court defer to an agency’s interpretation of a law,” says Bradner. He says there was a famous decision based around Chevron where the Court ruled that judges should not insert their interpretation of the statute in the place of the agency’s statute if the agency made the interpretation with a reasonable construction.
‘’Fast forward 35 years and a lot of the conservative jurists are questioning the Chevron decision…this very arcane question of calculating a fraction for the purposes of making Medicare payments to hospitals could serve as the basis for a significant change in the rules around judicial deference that would have an impact on all agencies and all manners of regulation,” Bradner adds.
What makes it potentially more impactful, Bradner adds, is that significant health care legislation is harder to pass in a more divided Congress. And even when it is passed, agencies like HHS are using interpretative language in current statutes to exert more authority and sometimes even bypass rulemaking processes. It is something that HHS even noted itself in a “Good Practices” rule it released in 2020 that clarifies guidance vs. rulemaking.
Bradner uses the ACA as an example of agencies having more of an impact in legislative interpretation. The death of former Massachusetts Senator Ted Kennedy forced the Democratic Congress to pass the ACA with “numerous ambiguities,” and it was left up to then-HHS Secretary Kathleen Sebelius to “do a lot of creative lawyering” to implement the law. The No Surprises Act, signed into law by President Trump in late December 2020, is a more recent example of this, Bradner says. He says it’s an extremely vague statute and there are issues within the law that were not addressed with granularity.
“In this day and age where it’s difficult to get agreement on the legislation and where Congress is often vague on key issues in order to bridge political differences, agencies have more and more been left to fill in the gaps. A change in that level of deference could create a lot of difficulties,” Bradner says.
Going forward, Bradner says that bigger regulatory changes are needed to better target DSH payments to hospitals who need it. He says the current definition of a DSH hospital included a large number of organizations, including ones that wouldn’t be thought of as a safety-net hospital.










