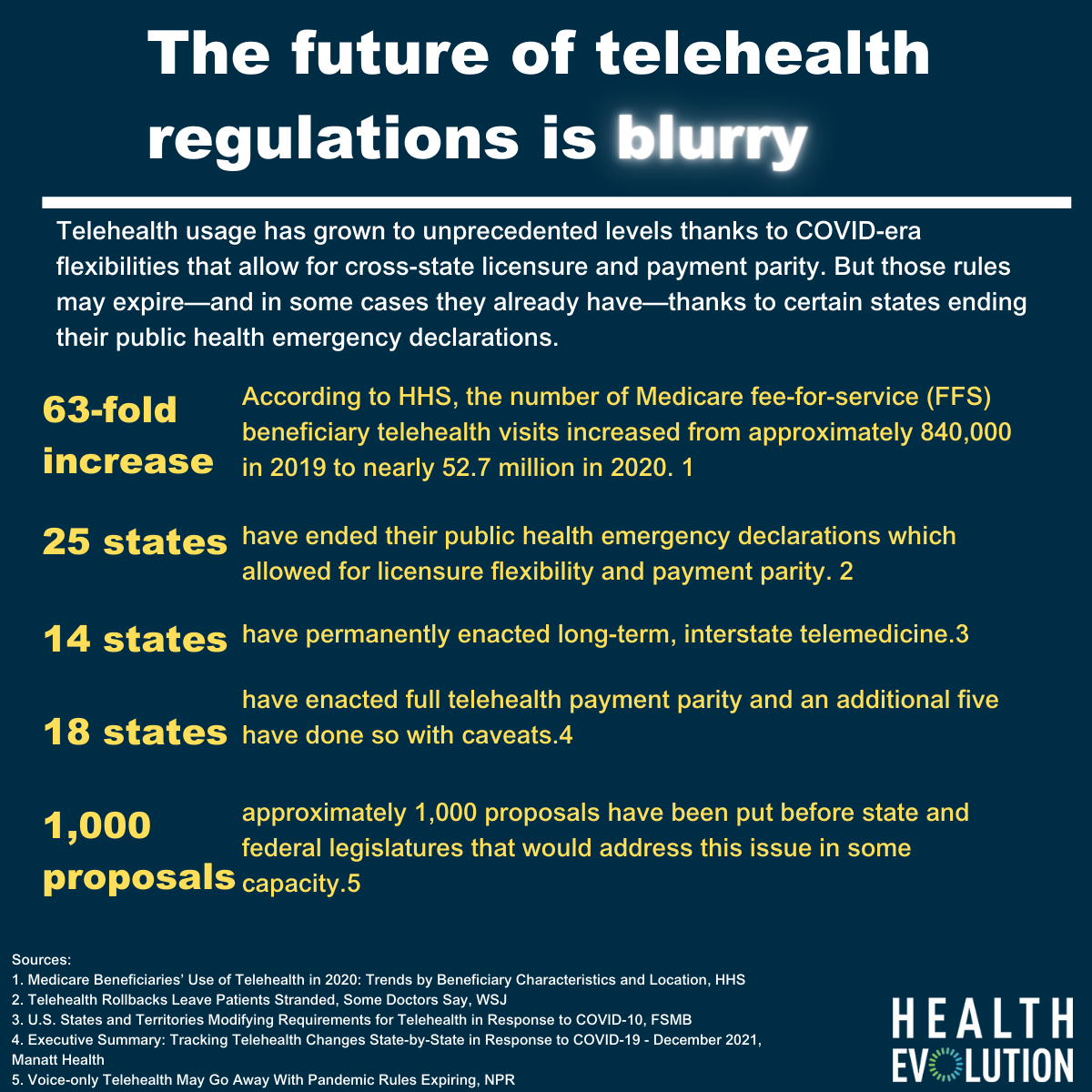
New data from HHS outlines how much of a phenomenon telehealth was in 2020 during the early stages of the COVID-19 pandemic. According to HHS, the number of Medicare fee-for-service (FFS) beneficiary telehealth visits increased 63-fold in 2020, from approximately 840,000 in 2019 to nearly 52.7 million in 2020.
While these numbers inevitably leveled off, there is concern among industry groups and stakeholders that they could sink back to pre-pandemic levels if Congress doesn’t act. This week, Ascension, Johns Hopkins, and a number of other prominent health care organizations launched a campaign to permanently end restrictions on telehealth that have been waived during the COVID-19 pandemic. The campaign, Telehealth Access for America, brought together 16 health care organizations urging Congress to keep pandemic-era telehealth flexibility rules in place forever.
“Protecting and expanding access to telehealth is essential to strengthening America’s health care future. Congress must act to expand patient choice in every American community, meet patients where they are, and bring health care into the 21st century. We owe it to our patients to make health care access easier, and patients with Medicare should not be excluded from this opportunity,” Brian Hasselfeld, MD, medical director of digital health and telemedicine at Johns Hopkins Medicine, said in a statement.
This push from the industry comes at a time when the future of telehealth flexibility is in flux. According to the Alliance for Connected Care via The Wall Street Journal, 25 states have ended their public health emergency declarations, which allowed for licensure flexibility and payment parity. Some states have made those rules permanent through their own legislation, but others have made the post-pandemic era of telehealth reimbursement and licensure rules less clear.
For instance, in Florida, Governor Ron DeSantis let the public health emergency expire and with that, flexibilities related to telehealth also expired. According to the Federation of State Medical Boards, “Out-of-state health care practitioners are no longer authorized to perform telehealth services for patients in Florida unless they become licensed or registered in Florida.”
FSMB also said that only 14 U.S. States plus four territories have permanently enacted long-term, interstate telemedicine. According to an analysis from Manatt Health, 18 states have enacted full payment parity and an additional five have done so with caveats. Only in those states will flexibilities around telehealth stay permanent—unless Congress passes a bill. In those states, private insurers are not required to offer payment parity.
At least one recently proposed bill, Creating Opportunities Now for Necessary and Effective Care Technologies (CONNECT) for Health Act of 2021 in the Senate, would address this issue. There’s also the Telehealth Expansion Act of 2021, which is a bipartisan bill sponsored by Senators Steve Daines (R-MT) and Catherine Cortez Masto (D-NV) and Representatives Michelle Steel (R-CA) and Susie Lee (D-NV). This would make permanent a waiver created by the CARES Act to allow Americans with Health Savings Accounts (HSA) to access telehealth services without first having to meet their deductible.
According to NPR, there are roughly 1,000 proposals before state and federal legislatures that would address this issue. More than anything, payment parity will be needed to keep the ball rolling on telehealth. Without payment parity, health care organizations aren’t getting enough from these services to cover even the cost of submitting the insurance claim. One option could be to increase the price consumers pay but that would likely mean decreased usage. A new study from RAND Corporation published in JAMA found that not surprisingly consumers are less interested in using telehealth if the out-of-pocket cost is higher than for in-person care.
“Patients may like telehealth in certain circumstances such as when they need care for minor health issues,” Zachary Predmore, the study’s lead author and an associate policy researcher at RAND, a nonprofit research organization, said in a statement. “But their willingness to use telehealth is very sensitive to costs. Patients may not perceive video visits to have the same value as in-person health care.”
RAND’s study found that people who preferred video visits were more sensitive to out-of-pocket costs than those who preferred in-person visits. People who prefer in-person care were willing to pay $20 more to do so than people who preferred telehealth.
Infographic sources:
Sources:
1. Medicare Beneficiaries’ Use of Telehealth in 2020: Trends by Beneficiary Characteristics and Location, HHS
2. Telehealth Rollbacks Leave Patients Stranded, Some Doctors Say, WSJ
3. U.S. States and Territories Modifying Requirements for Telehealth in Response to COVID-10, FSMB
4. Executive Summary: Tracking Telehealth Changes State-by-State in Response to COVID-19 – December 2021, Manatt Health
5. Voice-only Telehealth May Go Away With Pandemic Rules Expiring, NPR
Homepage image source: Photo by Tima Miroshnichenko from Pexels