Credit: Lyft Healthcare and Evidation
For patients living in underserved and vulnerable areas, transportation can be one of the most detrimental social determinants of health.
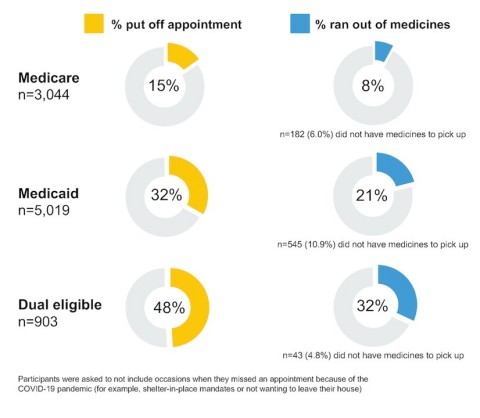
It especially has a long-term impact on patients who are on Medicaid and Medicare, according to a new study from Lyft Healthcare and Evidation. The companies polled 9,000 people across the country and found that 31 percent of dual-eligible beneficiaries missed provider appointments or ran out of medicine because they could not access transportation. These individuals were more likely to suffer from chronic conditions and mental illness, come from low-income households, and be under the age of 65, according to the research.
“A missed appointment or delayed care reduces the chances for early detection and prevention of health conditions before they worsen, threatening the long-term health of the individual and resulting in more costly interventions later, such as higher utilization of the emergency department, ambulances, and urgent care,” says Megan Callahan, Vice President of Healthcare at Lyft.
Lyft found that Medicaid and dual eligible beneficiaries miss appointments at double and triple the rates of Medicare beneficiaries and run out of medicine at triple and quadruple the rates of Medicare beneficiaries. Nearly half of dual eligible patients were putting off appointments due to lack of transportation and 32 percent ran out of medicine. Almost half of transportation insecure individuals surveyed are late to or needed to reschedule more than 10 percent of their health care appointments.
Health Evolution spoke to Callahan about the implications of these transportation challenges, what ROI can be expected from programs that address non-emergent care and how this problem factors into COVID-19 vaccine appointments. Below are excerpts from this interview.
For health care CEOs in the payer and provider world, what are some of the takeaways from the survey Lyft Health care did with Evidation?
It’s clear that one of the most common barriers to accessing health care is transportation, and the survey data adds new perspectives to the issue of transportation insecurity that can aid policymakers and key decision makers to develop action plans for this critical social determinant of health. The more data we can collect on how it affects specific communities and their needs, the more we can help in a very real way.
31 percent of beneficiaries surveyed missed appointments or ran out of medicine because they did not have transportation, and many of these individuals are more likely to suffer from chronic conditions or mental illnesses that require comprehensive care and consistent medication. And only 29 percent of Medicaid beneficiaries, for whom NEMT is a required benefit, are aware of their benefit. This tells us there’s a huge need for education among this population. This is especially important in a COVID-19 context, as more and more populations become eligible for the vaccine and low-income communities and seniors will face challenges with accessing transportation to vaccine sites.
What are the implications of 48 percent of dual eligible beneficiaries putting off appointments for non-emergent care?
This is a health equity issue, as those experiencing transportation insecurity are more likely to be lower income, people of color, people with disabilities, or the elderly. Medicaid and dual eligible beneficiaries are often the most vulnerable and can be the sickest adults in the health care system. A missed appointment or delayed care reduces the chances for early detection and prevention of health conditions before they worsen, threatening the long-term health of the individual and resulting in more costly interventions later such as higher utilization of the emergency department, ambulances, and urgent care.
What kind of ROI can be expected when health care organizations put into place programs to ensure Medicare and Medicaid efficiencies don’t fall into these transportation issues?
Transportation to and from appointments is a critical part of the care continuum, and when transportation is unreliable or unavailable, it often leads to delayed care and dissatisfaction with the health care experience. We’ve been working with our partners to study the impact of rideshare-based NEMT on health care access and quality for quite some time, and we know that Lyft can play an important role in helping communities live healthier lives. Organizations like AmeriHealth Caritas DC, Centene, and Amerigroup TN have reported improved health care utilization, better member satisfaction, and increased access to primary care. For example, after the implementation of Lyft within their NEMT program, AmeriHealth Caritas DC reported a 40 percent decrease in emergency room utilization, 15 percent decrease in low acuity non-emergent (LANE) ER utilization, 12 percent decrease in ambulance utilization, and 45 percent increase in compliance rate for 42 Health care Effectiveness Data and Information Set (HEDIS) measures.










