The future of the hospital pricing transparency rule is anything but certain.
While the rule was finalized earlier this year after it was upheld by the U.S. Court of Appeals for the District of Columbia Circuit in a December 2020 decision, few hospitals are compliant and data standardization issues persist among those that are.
The Trump-era rule requires hospitals to publish a “machine-readable” list of various charges for all items and services and a user-friendly list of prices for a smaller set of “shoppable” services. But so far hospitals have not really complied with the rule, according to an analysis from Kaiser Family Foundation. KFF found that only “35 of the 102 hospitals included in the analysis provide some payer-negotiated rates accessible to the public in a machine-readable file; only 3 provide payer-negotiated rates via consumer tools.”
Moreover, KFF found that even when hospitals were compliant, the lack of data standardization makes it difficult to compare prices across facilities. Another analysis from The Wall Street Journal found that many hospitals are hiding pricing data from their search results. Health Affairs also had a study on the lack of compliance to this rule. The American Hospital Association and other provider organizations have spoken out against it, arguing that it would divert resources away from the COVID-19 response.
Despite the pushback and lack of compliance from hospitals, CMS is moving ahead with pricing transparency, although with a different tact. As part of the Medicare Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospitals (LTCHs) proposed rule, CMS eliminated a requirement that hospitals had to report the payer-specific rates for inpatient services they negotiate with Medicare Advantage plans on their cost reports.
“We have long said that privately negotiated rates take into account any number of unique circumstances between a private payer and a hospital and their disclosure will not further CMS’s goal of paying market rates that reflect the cost of delivering care,” Tom Nickels, Executive Vice President of the AHA said in a statement, praising the agency’s decision. CMS did issue a warning notice recently to hospitals on noncompliance with the rule.
Political support
What’s working in favor of the pricing transparency movement is bipartisan support in an increasingly bipartisan political environment. Both Democratic and Republican leaders of the U.S. House Energy and Commerce Committee sent a letter to HHS Secretary Xavier Becerra imploring him to enforce the hospital pricing transparency rule.
“Given the widespread non-compliance by hospitals, we urge HHS to revisit its enforcement tools, including the amount of the civil penalty, and to conduct regular audits of hospitals for compliance,” wrote Chairman Frank Pallone, Jr (D-NJ), Ranking Member Cathy McMorris Rodgers (R-WA), Chairwoman of the Subcommittee on Health Anna G. Eshoo (D-CA), and Ranking Member of the Subcommittee on Health Brett Guthrie (R-KY).
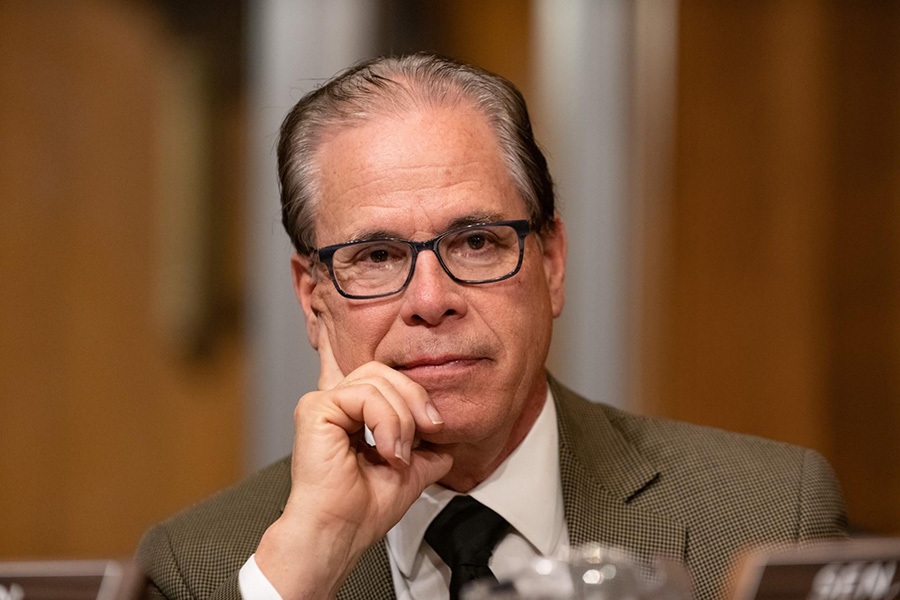
Indiana Senator Mike Braun spoke out adamantly in favor of pricing transparency and a free-market, consumer-driven health care system during a recent Kaiser Family Foundation webcast. As a former business executive, Braun described his experiences in reducing the cost of health insurance for his employees. He said he was tired of hearing how lucky he was that his health insurance costs were only going up 5-to-10 percent.
“The only way I could moderate premium increases was to bring in a new underwriter every three years to buy it down. My sized group was just large enough to self-insure, but we didn’t want to, and we were a high profit target for insurance companies,” Braun said. During a review of his insurance costs, he was told the biggest driver of costs was the “disengaged employed health care consumer. They are not interested in having any skin in the game.”
By investing in a consumer-driven health insurance plan, which has employees shop around for services, Braun says the company cut its health care costs in half. “I now have an employee base that’s doing everything they need to do [to find low-cost services] when they are engaged with the health care system, like they’re buying a big-screen TV,” he added. “Employees go less into their deductible now than they did 13 years ago because they are consumers of health care and they are price sensitive.”
Braun says this approach can work across the country but the reason it hasn’t happened yet is because “hospitals, [American Medical Association], pharma, insurance” are some of the biggest lobbyist groups in Washington. He says the Chamber of Commerce backs health care interests. Braun said transparency and competition needs to “bring the reins in.”
“What we have now is an unregulated utility,” Braun said. “Health care has the best of both worlds. They are an unregulated utility and many of my Senate buddies say they are in a free enterprise, which they are not.”