Earlier this week, enforcement of the ONC information blocking rule for providers within the 21st Century Cures Act took effect, and it will begin on July 1, 2021 for the CMS Interoperability and Patient Access Final Rule — both of which are reliant on the use of Application Programming Interfaces (APIs) for data sharing purposes.
Simply put: APIs are about taking data, making it liquid, and sharing it to deliver information into the hands of the right person to make decisions.
“There’s no way to do that without using APIs, which makes them mission critical,” said Gautam Shah, Vice President, Platform and Marketplace, Change Healthcare. Change Healthcare, in fact, released new research that found 9 in 10 executives (CEOs, CIOs, CTOs and others) consider APIs to be mission-critical to their business but only 24 percent use them at scale.
To that extent, here are aspects of APIs for CEOs to understand.
Health care has hit a regulatory inflection point relative to APIs
While the conversation about APIs in health care is not new, federal regulations are driving the urgency to adopt and implement APIs that enable information sharing. After talking about APIs and FHIR for some time now, the CMS and ONC rules are really the first impetus the industry has ever had to adopt and implement APIs. “We’re at an inflection point,” Shah said. “We as an industry do things when the regulatory forces require it.”
APIs provide an opportunity to rethink health care
APIs will naturally be deployed principally by IT, but how to leverage them strategically is not just a technology conversation and, instead, touches CMIOs, CNOs and other C-suite leaders as they can enable leaders to leverage APIs and embrace FHIR to drive interoperability, while focusing on what their department or the broader organization does well. “APIs are not bits and bytes,” Shah said. “APIs are enablers for executives to lead people to do their jobs better in every aspect of the ecosystem.”
APIs are the new lingua franca
COVID-19, particularly the related increases in telehealth utilization and aggregation of immunization data, has been a catalyst for APIs. But the ONC and CMS rules were underway well before the pandemic to enable care models in which consumers can choose providers, plans, care services and in certain cases house their entire medical history in their smartphones. This simply cannot be done without APIs that the industry embraces. Today, sharing a full medical record is the exception not the norm. “Now that APIs are regulated, that has turned them into a currency, you have to have them to communicate with each other organizations,” Shah said. “They are the lingua franca.”
APIs enable increased levels of patient experience and operational efficiency
By enabling everyone to have access to their health data, CMS is driving a combination of efficiency and care advancements. “If I can truly free this data, from a patient perspective I can do a better job sharing as much information as possible with the provider, not just a limited window into EHR data,” Shah said. “If I’m a CEO, I want to be able to provide the best data, best care, best operational efficiency.” That requires thought, deliberation and strategy. APIs can also extend organizations’ ability to improve business operations and run more efficiently by better leveraging appropriate information, Shah added.
Achieving more than minimum compliance can be a competitive differentiator — at relatively low incremental expense
Minimum compliance essentially means that the regulators will not come after an organization. Going above and beyond mere compliance with the ONC and CMS regulations, however, affords health care entities the opportunity to use APIs to establish points of competitive differentiation, Shah said. “If I can collaborate with outside organizations, operate at the right speed with the right reliability, security and privacy, I can enable all the ways we interact with the world today,” Shah said, citing online banking and retail as two examples. “The incremental cost of making that experience better is really low because you’re not developing it from scratch and speed to market is driven by that as well,” Shah said. “We’re no longer hampered by how much it costs to build competitive differentiators.”
APIs are a foundation on the path toward a better health care system
“The timing aspect of this is critical,” Shah said. “CEOs who haven’t started thinking about it yet should start now. Even if we don’t want things to be driven by enforcement, that is now the reality.”
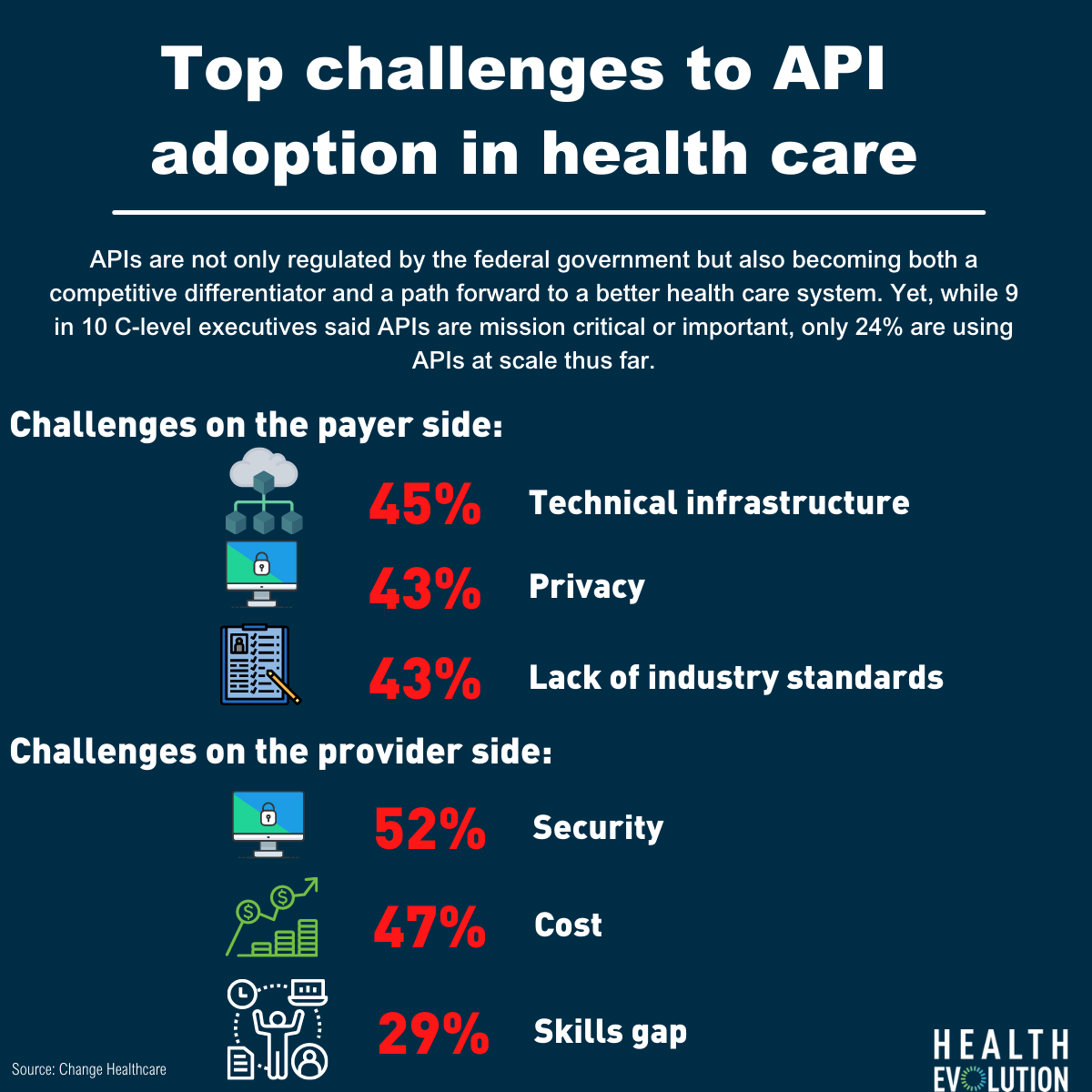
In the new research, Change Healthcare also found that 52 percent of providers identify security as the top challenge, followed by 47 percent listing cost concerns. Among payers, 45 percent said it is technical infrastructure, 45 percent privacy and 43 percent answered that lack of industry standards is a top challenge. The skills gap, meanwhile, is another issue with 35 percent of payers and 29 percent of providers saying experience creating APIs is a barrier.
Overcoming those barriers, by leveraging APIs and FHIR among other tactics, will be critical to improving and modernizing the health care system and the industry moving forward.
“The rise of APIs should be a great example of how clinical providers, non-clinical providers, technology teams, literally everyone can break the boundaries of data flow to partners and build the foundation for a better health care system,” Shah says.
Homepage photo credit: Canva bongkarn thanyakij