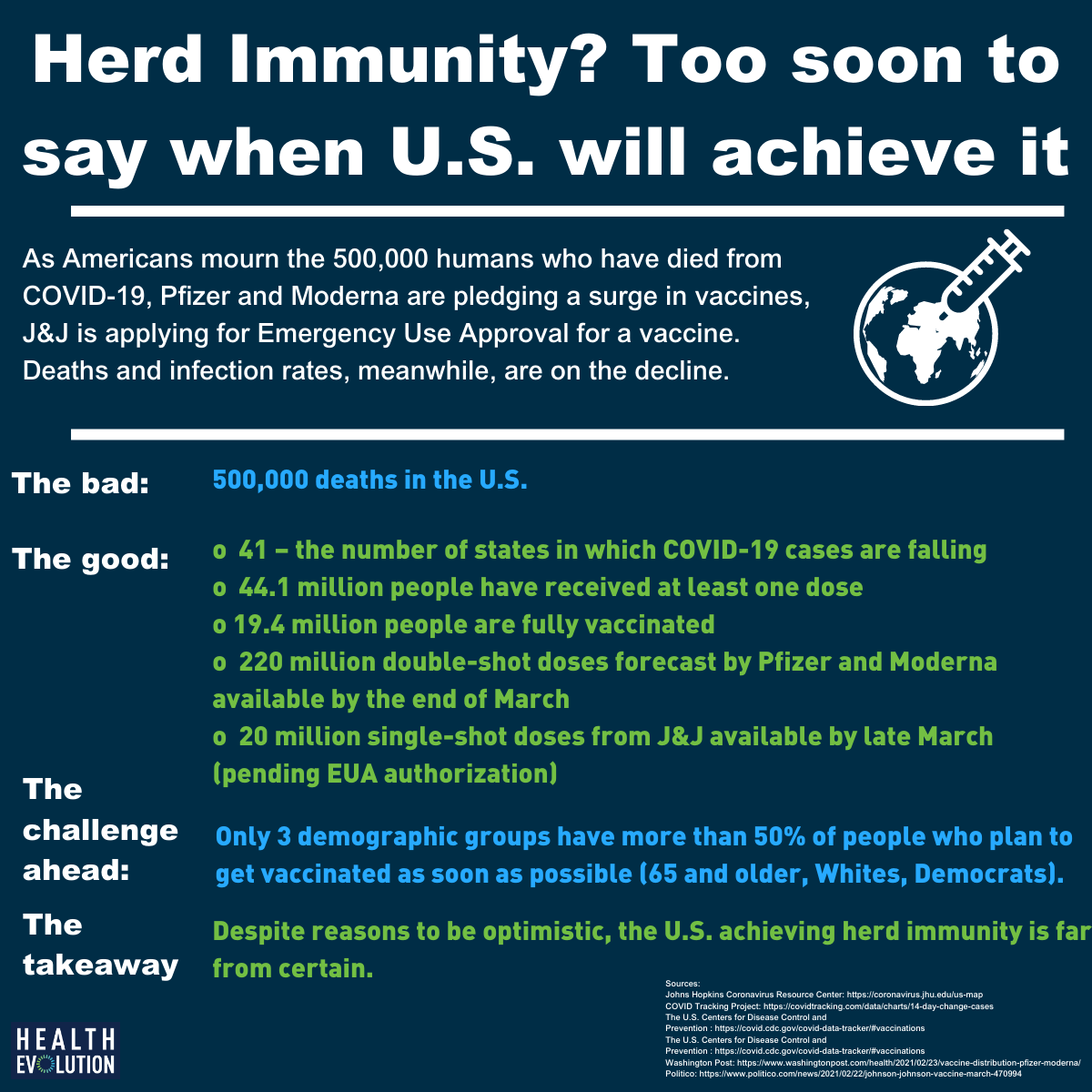
It’s a milestone of morbid proportions: The U.S. COVID-19 death toll surpassed 500,000 people amid a vaccine rollout that, at least to date, has been problematic. At the same time that Americans are mourning so many human lives lost to the pandemic, deaths and infection rates are on the decline and the availability of vaccine doses appear poised to surge in the weeks ahead — both of which illustrate the potential for the U.S. to approach a level of herd immunity necessary to re-open the economy.
But we do not yet have enough information to suggest exactly when the U.S. will achieve herd immunity, so let’s look at the data that is presently available.
Reasons to be optimistic: Deaths and vaccines
The U.S. is experiencing a 37 percent reduction in new cases and a 23 percent reduction in new deaths, the COVID Tracking Project, which calculates in 14-day increments, found as of February 23, 2021. And the Johns Hopkins Coronavirus Resource Center showed that COVID-19 cases are falling in 41 states.
What’s more, Moderna, which has thus far delivered 45 million vaccine doses, this week revealed plans to double the quantity it delivers to 40 million a month by April, according to the Washington Post, which also reported that Pfizer said it will increase the number it distributes weekly from 4-5 million today to 13 million by late March. J&J applied for Emergency Use Authorization for its vaccine, stating that it can produce 20 million single-shot doses by late March — and 100 million in the first half of this year. And on Wednesday, FDA scientists released new data showing that its vaccine has a 72 percent efficacy rate in the U.S. and 64 percent in South Africa.
That means potential exists to approximately double the 1.5 million doses being distributed daily. But as vaccine supply is increasing, distribution is encountering a significant obstacle.
Reality check: Vaccine hesitancy
The Kaiser Family Foundation’s COVID-19 Vaccine Monitor determined that only three of the demographics KFF tracks consist of more than half the people interested in receiving the vaccine now: 65 and older, Whites, Democrats.
The ongoing disparities in vaccine distribution are becoming increasingly clear even while California, Texas, and other states are redacting ethnicity and race information to withhold it from the U.S. Centers for Disease Control and Prevention, citing patient privacy rights.
“Across the 34 states reporting data on vaccinations by race/ethnicity, there is a largely consistent pattern of Black and Hispanic people receiving smaller shares of vaccinations compared to their shares of cases and deaths and compared to their shares of the total population,” according to the Kaiser Family Foundation. “White people received a higher share of vaccinations compared to their share of cases and deaths and their share of the total population in most states reporting data.”
All told KFF found that only 47 percent of Americans want to be vaccinated right away and that will make reaching herd immunity even more difficult — and serves as all the more reason for CEOs to advocate for vaccines.
Herd immunity: A matter of some debate
Late last week The Wall Street Journal published an opinion piece asserting that with cases down 77 percent from six weeks ago and some 150 million people projected to receive a vaccine by March’s end, “there is reason to think the country is racing toward an extremely low level of infection. As more people have been infected, most of whom have mild or no symptoms, there are fewer Americans left to be infected. At the current trajectory, I expect COVID-19 will be mostly gone by April, allowing Americans to resume normal life.”
The article sparked debate among epidemiologists, public health officials and prominent doctors firing back with one data scientist saying that models show theoretical immunity will not happen in 2021.
Striking a somewhat more middle ground perspective, former FDA head Scott Gottlieb, MD, told CNBC that vaccinating more people as the nation moves into warmer weather will lead to lower infection levels during spring and summer but that will not be the end of COVID-19.
“In the fall we’re going to have to take certain precautions, but we’re going to be back doing stuff. Then, as we get into the deep winter as this starts to circulate again, come December we may start to pull back,” Gottlieb said. “That doesn’t mean we’re going to have shutdowns but it means we might not have holiday parties, board meetings in December might be Zoom rather than in-person meetings.”
Related articles:
The politicization of vaccines and public health illustrates the depth of inequities
Public health messaging 101: How to convince the vaccine skeptics
Ad Council exec on COVID-19 vaccine campaign: ‘We are wired for crisis’
With public trust in COVID vaccines fading, health CEOs must be trust amplifiers
CEOs look to keep transforming health care in 2021
Homepage image credit: The U.S. Centers for Disease Control and Prevention