The COVID-19 pandemic has done a number on primary care—and it will continue to do so in the near future. In part one of our two-part series on COVID-19’s impact on primary care, our panel of experts shared the strains being put on doctors and independent practices alike.
“Primary care has been caught flat footed. A lot of these practices that on the fee-for-service, visit-based model are really struggling. That’s unfortunate because this is the time where good solid primary care should be having an impact, making sure patients at risk are kept safe and those who have needs are being addressed through virtual technology or otherwise,” said Scott Shreeve, MD, CEO of Crossover Health.
The experts also discussed what the financial closures of practices would do to the access of care in certain areas, the long-term impact on primary care and how the pandemic exacerbates existing issues of primary care.
In part two, we focus on solutions to the problem. What actions can health care organizations, specifically payers, take to sustain primary care both during and after the pandemic? What hope does the increased usage of telehealth offer primary care for the future? Our panel discusses all of this and more.
Panel of experts:
Farzad Mostashari, MD, CEO of Aledade, which partners with independent practices, health centers, and clinics to build and lead Accountable Care Organizations (ACOs); former National Coordinator for Health IT
Ateev Mehrotra, MD, associate professor of health care policy and medicine at Harvard Medical School
Christine Bechtel, president and chief strategist, X4 Health, a strategy consultant firm
Scott Shreeve, MD, CEO of Crossover Health, a digital health, national medical group
Chris Koller, Milbank Memorial Fund, an operating foundation that works to improve population health; former Health Insurance Commissioner of Rhode Island
What actions can health care organizations, specifically payers, take to sustain primary care?
Koller: I focus on payers because they are the ones with the one with the money. We have a collective problem in that if you go to any individual insurer, they know they need a strong primary care system. But no single insurer has enough business to change the finances of the primary care practice by themselves. If you think about it, primary care practices accept from Medicare, Medicaid and 10-15 commercial insurers. You need payers to act collectively to address the issues of primary care and preserve it in the long run. We’ve been looking at places where there are a small enough number of payers to make a difference. We’re also following a proposal from the Pacific Medical Group and California Medical Association, which are asking legislatures in the state to require health insurers to make $2.5 billion in prospective payments to independent primary-care providers for this year and next.
Mehrota: There have been a number of ideas proposed to help sustain primary care. The one that’s the most viable is prepayment. If I am a health insurer and I see based on prior data that I give $10,000 to a primary care practice for payment each month for the care they provide, what I’ll do is give them 80 percent of it to tide them over through the pandemic and ease their pain. It could be a lump sum payment or it could be as a conditional on visit patterns post pandemic. Those kinds of programs are helpful and important. We need more implemented between health insurers and Medicare. If these payers lose large primary care practices, it’s worse for their beneficiaries.
Mostashari: Payers should be thinking about which independent primary care practices are most important to you and how will you keep them healthy? Let’s face it, payers will have a surplus this year. Instead of paying them back because you exceeded your medical loss ratio, why don’t you spend some of that on primary care? And do it in a way that sets primary care on a track towards person-based, longitudinal payments, towards value-based care. We see too many people not making a move. “Let me just hold on to this cash because I don’t know what’s going to happen.” You know what’s going to happen. Some of these practices will go out of business and you’ll be in worse shape down the line. Payers need to use long-term thinking and long-term actions. 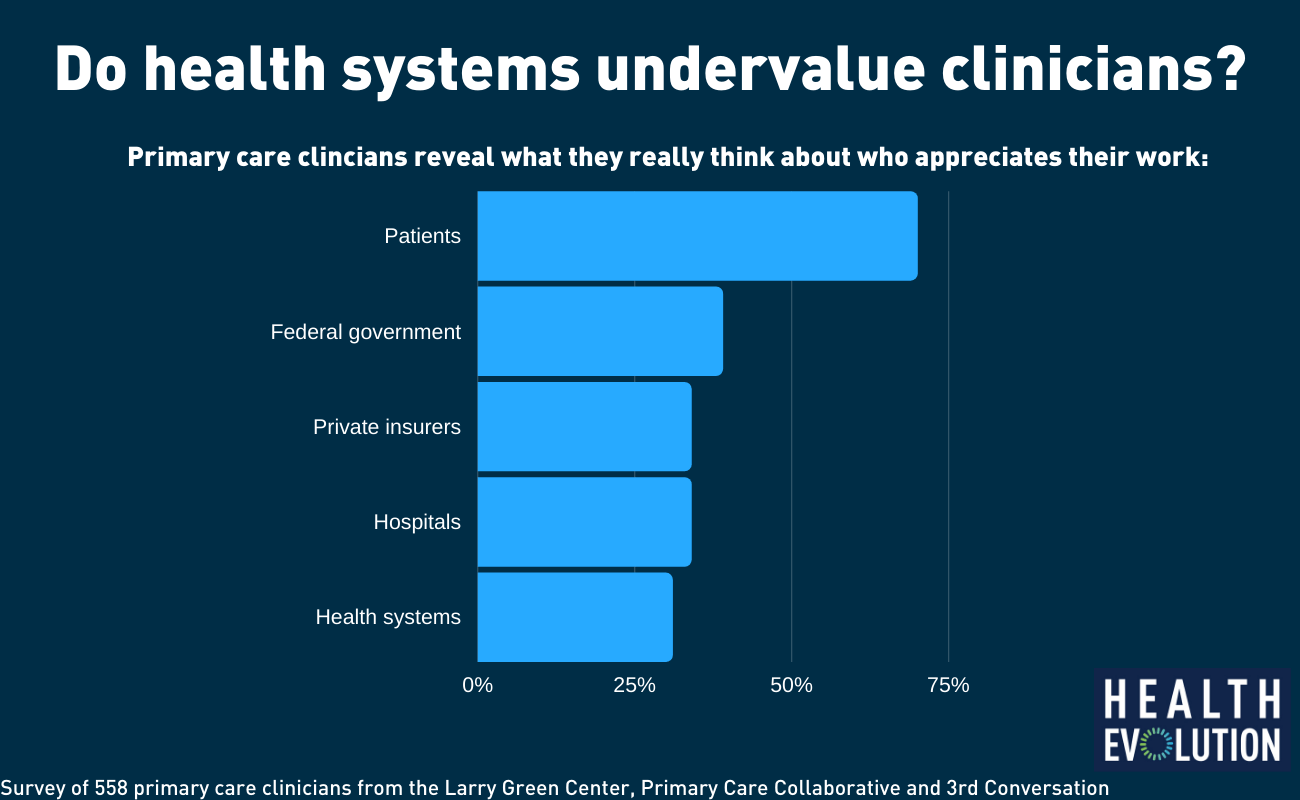
Bechtel: There is an immediate role in injecting stabilizing funds and there’s a longer-term role for payers to play. Unfortunately, primary care practice, based on our survey data, are telling us the commercial payers are not doing a great job of paying for telemedicine. Not all are doing pay parity and 20 percent of practices are seeing denials of the bills they’ve submitted to commercial insurers. There’s definitely an opportunity for private payers to do better. We asked primary care practices who they feel valued by. Seventy percent feel valued by their patients. That’s awesome. Patients are allies. Only 39 percent felt valued by private insurers. That’s a huge delta with how these practices feel valued by patients vs. commercial and government insurers.
What hope does the increased usage of telehealth offer primary care for the future?
Shreeve: Most people think of virtual care as some kind of video visit done over the internet. We find that only a small percentage of virtual visits are done that way. Most people just want to get in touch with their doctors. The most common way is over the phone. If you look at some of Teladoc’s numbers, there are a ton of telephone calls because that’s a normal, convenient way to get in touch with a doctor. Video visits are interesting and there are certain cases where that’s effective. Most of what we see is asynchronous communication. People want to text and message their provider quickly and then thoughtfully write comments as needed. The approach Crossover took, and where we think the bulk of telehealth will go, is the ability to stay connected to the patient. And most people want to text or message their provider.










