In this series, Health Evolution is examining the year 2021 in health care through the lens of our eight imperatives. We will be examining the trends that were at the top of CEOs’ minds throughout the past year and what may come in 2022. This week: Realizing medical breakthroughs
Previously:
Strengthening system resilience
Confronting the mental health crisis.
For cancer patients, COVID-19 has been brutal.
A recent study from Dana Farber Cancer Institute found that even fully vaccinated cancer patients with breakthrough COVID-19 infections had a hospitalization rate of 65 percent, an ICU or mechanical ventilation rate of 19 percent, and a 13 percent death rate. Comparatively, recent data from New York State shows that only .15 percent of all fully vaccinated people were hospitalized.
“Patients with cancer who develop breakthrough COVID-19 even following full vaccination can still experience severe outcomes, including death. That is why a multilayered approach that includes masking and social-distancing, along with vaccination plus booster against COVID-19 remains an essential approach for the foreseeable future,” stated Toni Choueiri, MD, director of the Lank Center for Genitourinary Care at Dana-Farber Cancer Institute.
Another research effort, from the National Cancer Institute, found that patients with cancer are at increased risk of severe COVID-19 disease. NCI also found that hospitalized cancer patients have a severe disease course and a high mortality rate.
Health Evolution Summit 2022, April 6-8, Laguna Niguel, CA: Apply to Attend
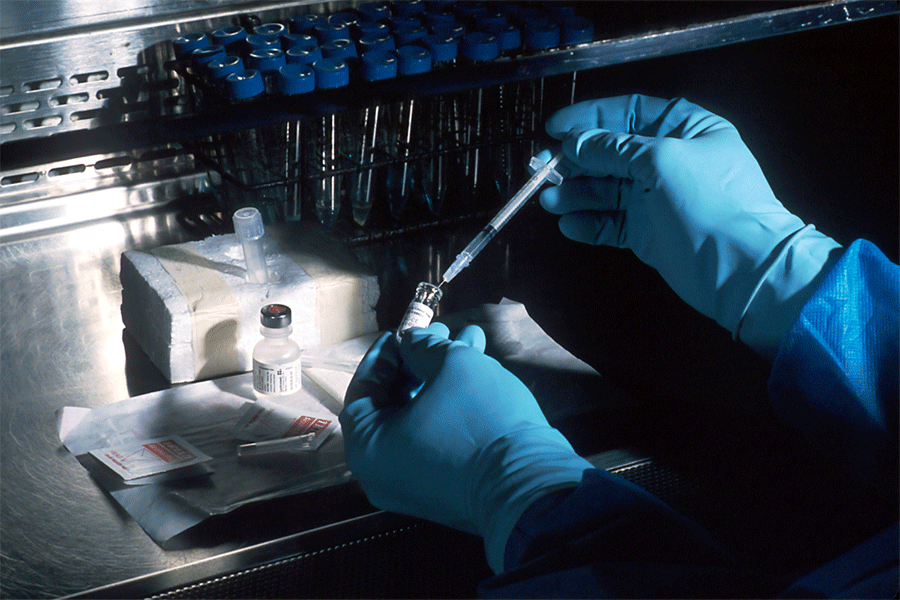
But amid the harsh reality that COVID has brought to cancer patients, there is hope coming within the oncology world. The quick development of messenger RNA (mRNA) vaccines used against COVID-19 has given renewed emphasis on using the technology to increase the speed of approval for cancer treatments.
In a recent survey by research firm PureSpectrum and real-world data and analytics company COTA, 71 percent of oncologists say patient expectations for faster development of new cancer treatments have increased because of the perceived speed of COVID-19 vaccine development. While 64 percent of oncologists are satisfied with the pace of typical cancer treatment clinical trials, they understand that there is an opportunity to improve the process through the use of real-world data.
“Everyone understands that we can be more efficient with clinical trials. The pandemic highlighted the vital benefit that real-world data has when it comes to ensuring efficacy and safety for development of therapeutics,” says Andrew Pecora, MD, founder of COTA and former president of Cancer Services at the John Theurer Cancer Center at Hackensack University Medical Center. The Centers for Disease Control and Prevention (CDC), among other entities, published data that signified the benefits of the mRNA COVID-19 vaccines using real-world data, rather than traditional clinical trial data.
“With real-world evidence, we’ve shown that you don’t need a control group. If you don’t need a control group, you can use people in the real world, trial times will be cut in half, the time to complete trials will be cut in half, the cost will be cut in half and most importantly, people in the control group are not going into a study that has no potential of benefitting them more than the standard of care,” Pecora adds.
The future of mRNA vaccines and cancer
While most people likely have not heard of mRNA vaccines before the COVID-19 pandemic, they are not new. The history of the technology dates back to the 1960s. The first mRNA flu vaccine was tested in the 1990s and there was an mRNA rabies vaccine tested in 2013. Meredith McKean, MD, MPH, Associate Director, Melanoma and Skin Cancer Research, Sarah Cannon Research Institute at Tennessee Oncology, says mRNA cancer vaccines have been in clinical development for five years at her organization.
“COVID has shined the spotlight on mRNA vaccines and cancer. There are a number of different immune therapies ongoing and clinical trials trying to make progress for patients with both localized cancer…and for patients in the metastatic setting. Although mRNA technology was already in development with cancer, it’s given a nice spotlight to the ongoing work and brought more interest from patients who want to participate in those studies,” says McKean.
BioNTech, which produced one of the COVID-19 vaccines alongside Pfizer, is currently in the trial stage for a mRNA vaccine that can treat patients with anti-PD1-refractory/relapsed unresectable Stage III or IV melanoma. The company also has another trial for a potential vaccine that would treat stage II/III colorectal cancer patients. The revenue it receives from the COVID-19 vaccines will help further the cancer vaccines within its mRNA platform, according to BioNTech CEO Uğur Şahin.
We have better medications that have much less side effects, or different side effects that can be managed much easier, and patients are living longer with their disease. I hate the expression ‘patients are dying with their cancer,’ because they’re living with their cancer and we want to continue to allow them to live.
Roger Brito, DO, CVS Health
“We now have the funding to accelerate our cancer pipeline and make it even bolder. It’s not that we are shifting resources, but rather that we can now be much bolder than we were before,” Şahin said to Nature.
Thanks to the success of the COVID-19 vaccines, McKean expects there to be a lot of developments related to mRNA cancer vaccines in 2022. She says there will be studies that will finish accruing in both the metastatic and adjuvant settings. Along with melanoma and colon cancer, there are mRNA vaccines being developed for different tumor types. She says she is excited to see the data to see if these mRNA vaccines are beneficial, in what setting, for which tumor types, and when they should be used.
Challenges ahead
What’s potentially challenging for the development of mRNA vaccines for cancer is what makes it a huge opportunity: The fact that cancer treatment requires more personalization. McKean says that the expectation is that every patient, particularly in a metastatic setting, can have full molecular profiling to determine the specific drivers of that patient’s cancer.
“mRNA vaccines are an exciting opportunity to personalize cancer treatment for patients, the challenge is any time you are personalizing something and trying to get more information for specific patients, it can take more time,” says McKean. “This has been a challenge for a long time, looking to develop vaccines for common cancer antigens. They just weren’t specific enough and didn’t see responses.” She adds that while mRNA vaccines can cutdown the time it takes to personalize treatments, , it still takes longer than an off-the-shelf treatment option.
More personalized treatments also mean higher costs, not just for the development of mRNA vaccines but many of the other breakthrough therapies associated with cancer, says Roger Brito, DO and the Divisional Head of Enterprise Oncology at CVS Health. “I’ve been in practice for 25 years and I used to talk about how expensive drugs were when they cost thousands of dollars. Today, it’s hundreds of thousands of dollars in a relatively short period of time, a decade and a half. With advanced technology and better drugs, we’re certainly now having to focus on cost containment,” Brito says.
Brito says analytics driven approaches can help providers effectively find the most appropriate standard of care and lower the cost. CVS Health has a program, Transform Oncology Care, which includes a platform that uses real-time guidelines for cancer treatment and integrates it into an oncologist’s workflow. This can help reduce the number of tests that a patient has to endure and the timeline for treatment plans, and it can also reduce hospitalizations for side effects, which is particularly ideal in the time of COVID.
“If you have a weakened immune system, the last place you want to be is a hospital,” says Brito. “That has always been the case, but it’s especially the case right now thanks to the pandemic.” Of course, this approach itself is not without its own challenges. He notes that integrating these guidelines into an oncologist’s practice isn’t always seamless because providers and patients will have different needs. Like everything else related to cancer care, Brito says that solutions must be nimble enough to customize for the particular circumstance.
Despite the challenges outlined above with cost and customization, there is plenty of optimism to go around. Advances in cancer treatments have already come a long way in decreasing the cancer death rates. mRNA technology and other breakthrough therapies can push these numbers to an even better place.
“I’m 1,000 percent optimistic. I’ve been practicing oncology for 25 years and back then, I couldn’t tell you that if you had metastatic non-small cell lung cancer, you could live for an average of 24 to 36 months. It was 8-10 months, 25 years ago. People are living longer with their cancers,” says Brito. “We have better medications that have much less side effects, or different side effects that can be managed much easier, and patients are living longer with their disease. I hate the expression ‘patients are dying with their cancer,’ because they’re living with their cancer and we want to continue to allow them to live.”